To answer key questions on the impact of COVID-19 for patients with CML and to help physicians confidently treat people with CML during the pandemic, the iCMLf has collected and analysed COVID-19 cases among patients with CML globally.
The full case summary comprises a total case number of 1,056 COVID-19 and CML cases submitted from 177 institutions in 57 countries and 205 physicians, and represents the largest global cohort of CML patients with COVID-19.
'The iCMLf CANDID study gave confidence for physicians worldwide that their patients with well controlled CML were not at greater risk from COVID-19 than the general population and no changes to CML therapy specifically due to SARS-CoV-2 infection were required.’ (Professor Jorge Cortes)
Below we summarise the key data that have been presented at major meetings from this important registry.
We are delighted to share that the final results of the iCMLf CANDID study will be presented as a poster at the EHA2024 Hybrid Congress.
 Coming soon:
Coming soon:
EHA 2024: COVID-19 in patients with CML:
Final results from the global observational iCMLf CANDID Study
Poster to be presented at the European Hematology Association (EHA) Hybrid Congress 2024 (Réa D et al.)
Poster session: Chronic myeloid leukemia - Clinical
Date: Friday, June 14, 2024 from 18.00 - 19.00 CEST (Poster Area, Hall 7)
Aim: The study delves into the impact of COVID-19 on patients with CML globally.
Conclusion: The majority of CML patients experienced mild/moderate forms of COVID-19. The COVID-19 severity/mortality rates for patients with CML were lower compared to other hematological malignancies. Factors such as age, comorbidities, and CML phase influenced COVID-19 outcomes.
This research underscores the importance of vaccination for CML patients, emphasising its role in reducing individual risk and disease transmission.
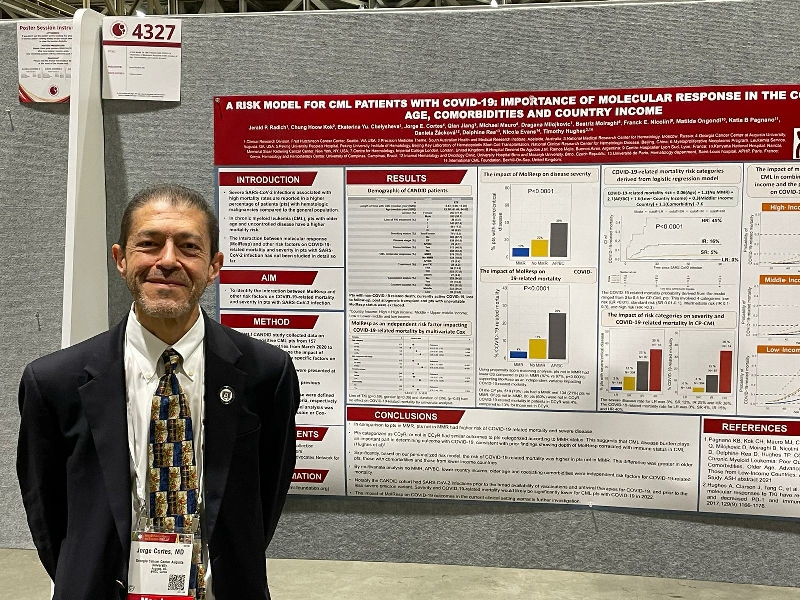 ASH 2022: A risk model for CML patients with COVID-19:
ASH 2022: A risk model for CML patients with COVID-19:
Importance of Molecular Response in the context of age, comorbidities and country income
Poster presentation at the American Society of Hematology (ASH) Meeting 2022
(Radich J et al).
Aim: To identify the interaction between molecular response and other risk factors on mortality and severity in patients with SARS-CoV-2 infection.
Conclusion: Based on our personalized risk model, the risk of COVID-19-related mortality was higher in patients not in MMR. This difference was greater in older patients, those with comorbidities and those from lower income countries.
Read the full abstract here
John Goldman Conference on CML 2022:
Subanalysis of patients with COVID-19 and CML on TKI treatment
Poster presentation at the John Goldman Conference on CML: Biology and Therapy 2022
(Prado A et al.)
Aim: This subanalysis of the CANDID study investigated the role of tyrosine kinase inhibitors (TKI's) on clinical evaluation and outcomes in patients with COVID-19 and CML. Severity and mortality of COVID-19 was analyzed according to age, type of TKI, line of treatment, disease stage, TKI response, treatment interruption during infection, standard or modified dose of imatinib, and number or comorbidities.
Conclusion: Survival of COVID-19 in patients with CML on tyrosine kinase inhibitors is remarkable high and there is no difference within the type of TKI, supporting that it is safe to maintain TKi treatment during COVID-19 infection.
EHA 2022: COVID-19 in patients with CML in treatment-free remission (TFR):
Disease severity and impact on TFR status
Abstract presented at the European Hematology Association (EHA) Congress 2022 (Saußele S et al.)
Aim: This sub-analysis of the CANDID study aimed to evaluate the outcome of SARS-CoV-2 infection in CML patients in treatment-free remission and assessed any impact on maintenance of TFR. Additional information were collected for this analysis including: molecular remission status before, during and after COVID-19 infection.
Conclusion: In this subanalysis of the CANDID study, CML patients had similar severity and survival to CML patients who were on TKI therapy and there was no evidence of an increases risk of TFR loss after SARS-CoV-2 infection.
Read the full abstract here
ASH 2021: An update of the CANDID study: Poor outcomes for patients with comorbidities, older age, advanced phase disease, and those from low-income countries
Oral presentation at ASH 2021 (Pagnano K et al.)
Aim: This update of the CANDID data explored the impact of various risk factors, such as co-morbidities, age, disease phase, CML treatment and economic status of the country of origin on clinical outcomes.
Conclusion: The analysis based on 642 cases of COVID-19 reported from 49 countries confirmed a higher mortality for CML patients with COVID-19 in older patients (>75 years), patients with cardiovascular or pulmonary comorbidities and from low and low-middle income countries, the latter probably related to limitations in supportive care. Additionally, more deaths occurred in patients in advanced phases and in patients not in MMR. CML treatment and line of TKI therapy did not influence the COVID-19 outcome.
ASH 2020: COVID-19 in patients with chronic myeloid leukemia (CML): Results from the International CML Foundation (iCMLf) CML and COVID-19 (CANDID) Study
(from March 12, 2020 as of July 1, 2020, 110 cases)
Oral presentation at ASH 2020 (D Rea, et al)
Aim: To rapidly collect and analyze information on COVID-19 cases among CML patients to define prognosis, risk factors and outcome. Defining risk and predisposing features in CML patients could guide interventions, therapy modifications, and clinical management for patients and physicians.
Conclusion: Currently, the mortality rate from COVID-19 in evaluable CML patients is 13.7%. Factors associated with a higher mortality rate are age and imatinib therapy. Imatinib may represent a confounder as opposed to a true adverse prognostic predictor given the strong link between imatinib treatment and advanced age. Further case reports and longer follow up are needed to better ascertain independent risk factors, the impact of COVID-19, and the possible role that TKI type may play in this population.
This huge endeavour would not have been possible without a truly global collaboration. We like to sincerely thank all the 200 physicians who contributed data.
Sincere thanks also go to Novartis Oncology and Pfizer for study funding.
We acknowledge and thank our partners The Max Foundation and CML Advocates Network for their support with case collection.










