 An editorial by Lisa Machado from the Canadian CML Network
An editorial by Lisa Machado from the Canadian CML Network
It’s time to stop equating survival with quality of life
Feeling so fatigued that you can’t work, maintain a social life or do the things that bring you joy is not living
If you are someone who has the good fortune at this moment in time to not be living with an illness, or caring for someone who is, lean in: survival and quality of life are not the same things.
Certainly, faced with a choice between dying or living, most of us would gratefully choose the latter without taking a breath. In fact, that feeling of fear and the desperation to live — also felt by those who love us — is often overwhelming, crowding out any contemplation of what the living that we are holding out for will look like.
But what happens when this new kind of “living” is nothing like the life you had before diagnosis? When your body is fatigued and in pain, when the vomiting and nausea comes daily, your mind is foggy with anxiety and depression, and any energy or will to do the things that bring you joy have evaporated? And what if, amid all this upheaval, your doctor — and maybe your family and friends, too — don’t really see your struggle, referring to your disease as “lucky,” your living “fortunate,” and breath, something to be grateful for.
This challenging state of being is all too familiar for many people living with serious health issues. From cancer and mental health to cardiovascular and neurological conditions, patients with diseases that have treatments often face an unexpected fight of their lives: to live well with their disease.
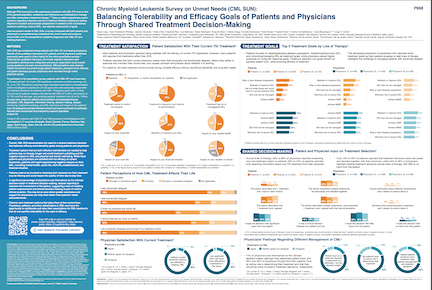
Living well despite your diagnosis has long been a hot topic within the CML community, but no more so than with the recent release of the findings of the CML Survey of Unmet Needs (SUN), a global patient and physician survey by Novartis Oncology. (In a game-changing move, the dissemination of the survey data, which recorded the responses of 361 patients and 198 physicians in 11 countries, was led by the CML community, using patient and caregiver voices to translate the findings through the lenses of lived experience).
Watch patient and clinician videos and read patient stories here
With the release of the survey findings came a collective sigh of relief from people living with CML and their caregivers. Finally, we were speaking out loud on a global platform about what we have known to be true all along: that although we are fortunate to have medication that gives us the best chance of surviving a disease that was once a death sentence, many of us don’t have an opportunity to truly enjoy this gift because of burdensome side effects. In fact, according to the survey findings, although most patients said they were satisfied with the effectiveness of treatment, they also reported that their lives were negatively affected by physical and emotional fatigue that limited their social and personal lives, the ability to exercise and caused them to take time off from work. In addition, they worried about treatment affordability and efficacy.
That the effects of treatment negatively impact emotional and mental health, as well as limit physical ability, are concerning issues in themselves. After all, we know that people who experience life-affecting side effects are less likely to take their medication the right way — or take it at all. But perhaps more worrying were the insights and opinions of doctors, particularly in terms of the assumptions they make about a patient’s treatment goals (focusing on response) and their perceptions of the role (almost none) patients should play in the decisions about their care.
Consider these findings from the survey: of the doctors who participated, molecular response was their top goal of treatment, whereas patients — while also focused on stopping/slowing progression of the disease — prioritized minimizing side effects and maintaining a good quality of life. And while the survey found that most doctors believed patients should be more involved in treatment decisions, almost three-quarters of those who participated considered themselves the ultimate decision-maker. These last two results beg a very important patient care question: how can we possibly get care that meets our needs and expectations if our doctors don’t understand our treatment goals or regard us as partners in our care?
Well, we can’t.
So what now? Clearly, the CML SUN results have kicked off a very important discussion around the unmet needs of CML patients, many of which are tightly tied to the onerous gaps in communication that exist in the relationships with doctors. Moving forward with an eye on improving the quality of life for patients, the responsibility to make serious change happen seems to lie with both doctors and patients. For doctors, it means a shift away from focusing on just numbers to seeing patients as whole beings with individual hopes and expectations around what living well with CML means to them and working together to get them as close to this ideal as possible. For patients, it means getting educated on treatment options, learning how to communicate expectations and goals clearly to doctors and being unwavering in the quest to achieve the best possible quality of life.
After all, patients deserve more than just to survive — they deserve to thrive. And we can get there with access to therapy options that are effective, yet tolerable, and treatment decisions that are made together with doctors, as partners.
Click here to find more information on the CML SUN Study
Lisa Machado is the founder of the Canadian CML Network. She also led the development of the CML SUN advocate page that features interviews with patients and doctors exploring their thoughts on the survey findings.










